Sickle cell disease (SCD) is one of the most complex conditions in the field of genetic disorders. Each type reveals a slightly different story, resembling a mosaic of inherited mutations; some whisper of tolerable pain, while others roar with urgent, life-threatening complications. But amid the hardship, there is a story of incredible medical progress and the fortitude of those impacted.
Research and treatment options for sickle cell disease have significantly improved over the last ten years. Through the use of stem cell transplants and gene therapy, medicine is gradually removing what was once an inflexible diagnosis. It’s important to comprehend the various forms of sickle cell disease and what each means for those who have it before discussing treatments and advancements.
Major Types of Sickle Cell Disease
| Type of SCD | Genetic Makeup | Severity Level | Key Characteristics |
|---|---|---|---|
| Hemoglobin SS (HbSS) | Two sickle cell genes (S from both parents) | Most severe | Chronic anemia, frequent pain crises, higher complication risk |
| Hemoglobin SC (HbSC) | One sickle gene (S) + one C gene | Moderate | Less severe than HbSS but still impactful |
| HbS Beta Thalassemia (β⁺) | One sickle gene + mild beta-thalassemia gene | Mild to moderate | Reduced beta-globin leads to mild symptoms |
| HbS Beta Thalassemia (β⁰) | One sickle gene + severe beta-thalassemia gene | Severe (like HbSS) | No beta-globin, similar symptoms to sickle cell anemia |
| Hemoglobin SD, SE, or SO | One sickle gene + one rare variant (D/E/O) | Rare and variable | Symptoms range from mild to severe |
| Sickle Cell Trait (HbAS) | One sickle gene + one normal gene | Asymptomatic carrier | No disease but can pass gene to children |
Hemoglobin SS: The Aggressive Architect of Anemia
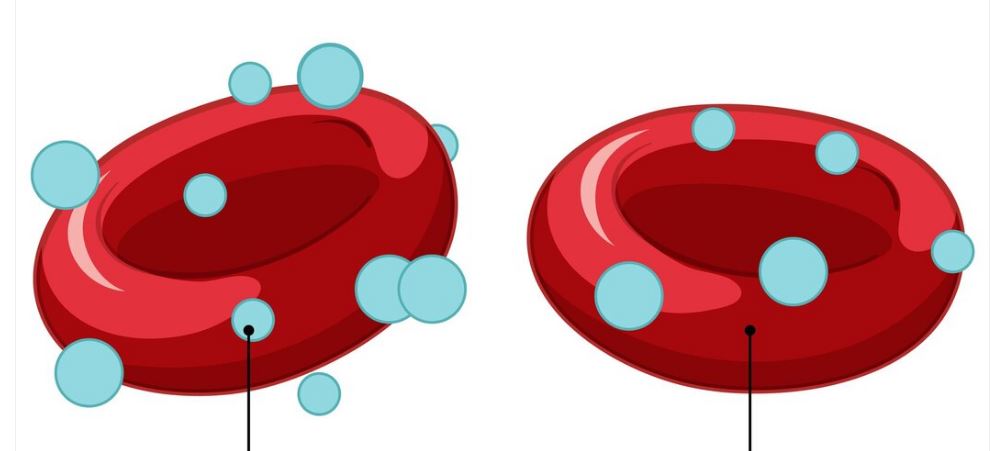
The most common and severe type of sickle cell disease is hemoglobin SS (HbSS), also referred to as sickle cell anemia. Surprisingly, it represents roughly 65% of all cases. Nearly all hemoglobin is abnormal if the “S” gene is inherited from both parents. Red blood cells twist into rigid, crescent shapes as a result, obstructing vessels and causing excruciating blockages.
Fatigue, persistent anemia, and recurrent hospitalizations are common in children with HbSS. However, their quality of life has significantly improved due to early diagnosis and proactive care. Today, hydroxyurea, a drug that lessens sickling, is changing results, and newborn screening programs detect the illness early.
Milder but Still Demanding Hemoglobin SC
One could refer to hemoglobin SC as HbSS’s “quiet cousin.” It develops when the S gene is contributed by one parent and the C gene by the other. Despite being categorized as moderately severe, this form has a surprising amount of impact. Although there are fewer pain episodes, splenic damage, joint problems, and vision problems are still major worries.
Many patients, especially those who receive a diagnosis during adolescence, may experience SC disease as an erratic visitor that is occasionally quiet and occasionally noisy. Effective management of these sporadic flare-ups is aided by targeted medication, regular checkups, and adequate hydration.
Sickle Cell and Beta-Thalassemia: A Complicated Partnership
A sickle gene and a thalassemia gene are combined to cause this type of sickle cell disease. The outcomes? a wide range. The person still has some capacity to produce normal hemoglobin if it’s the “plus” form (HbSβ⁺), which helps to control symptoms. However, if it is “zero” (HbSβ⁰), it resembles HbSS in severity, including anemia, organ stress, and pain.
This group is especially interesting from a clinical perspective. Because it has significantly fewer healthy red blood cells and frequently necessitates ongoing transfusions, the “zero” subtype is particularly difficult. Even so, novel treatments—such as gene-editing techniques that are presently being researched—offer encouraging avenues for advancement.
Hemoglobin SD, SE, and SO are uncommon but real.
SCD can occasionally show up in more unusual genetic combinations. Hemoglobin SD, SE, or SO diseases can be caused by inheriting the sickle cell gene in addition to D, E, or O variants. Although much less frequent, these disorders have the same risk of vascular problems and red blood cell deformation.
It may take longer to diagnose people with these less common types, and specialized genetic testing is frequently necessary. However, once recognized, treatment approaches are similar to those of more prevalent types, emphasizing symptom control and preventing complications.
The Silent Carrier with a Strong Legacy: The Sickle Cell Trait
Despite not being a disease, sickle cell trait (HbAS) is an important aspect of the narrative. One normal gene and one sickle gene are inherited by those who possess the trait. Although they rarely exhibit symptoms, they may have minor complications in extreme situations, such as severe physical exertion or dehydration.
They are carriers of genes, which is more significant. A child born to two carriers has a 25% chance of inheriting sickle cell disease. Genetic counseling becomes especially helpful for family planning in this situation.
Gene Therapy and Beyond: A New Era in Therapy
Gene therapy is predicted to transform treatment in the upcoming years. Scientists hope to offer a one-time fix rather than ongoing care by directly repairing the defective hemoglobin gene within stem cells. According to preliminary findings from clinical trials, some patients have been symptom-free for years after treatment.
In the meantime, drugs like crizanlizumab and voxelotor are decreasing anemia and pain crises in day-to-day living. Pharmaceutical companies and research institutions are collaborating strategically to develop targeted solutions that were previously thought to be unattainable.
Hope for the Future
In the past, sickle cell disease in all of its manifestations seemed to be an irreversible punishment. However, science is altering that narrative with its inventiveness and compassion. In addition to treating symptoms, we are rewriting futures as we gain a deeper understanding of the disease’s complex variations.
Those born with sickle cell disease today have a very different outlook than they did a generation ago thanks to individualized care, genetic insight, and a strong international community. And that is definitely cause for celebration.