Home
What is Sickle Cell Anemia
The discourse surrounding sickle cell anemia has changed in recent years from pessimistic predictions to optimistic realities. This hereditary disorder was once thought of only as a crippling, lifelong burden, but it is now being treated with incredibly effective therapies and innovative care approaches.
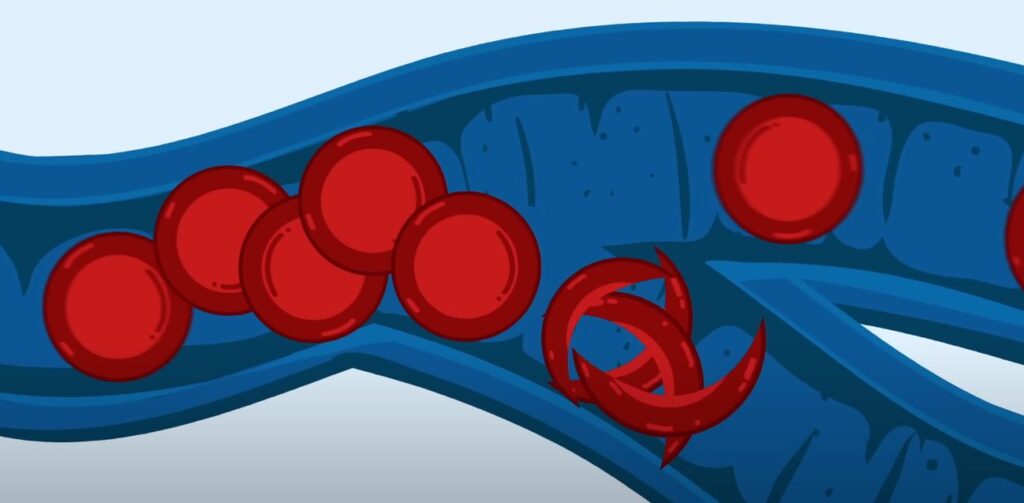
Fundamentally, sickle cell anemia is a genetic blood condition in which red blood cells become rigid and crescent-shaped instead of round. Blood vessels become similarly obstructed, limiting the delivery of oxygen and causing excruciating crises, much like a freeway jammed with twisted cars.
| Attribute | Description |
|---|---|
| Condition Name | Sickle Cell Anemia |
| Type | Inherited Blood Disorder |
| Cause | Mutation in the HBB gene affecting hemoglobin |
| Red Blood Cell Shape | Crescent or “sickle”-shaped instead of round |
| Main Problem | Blocked blood flow leading to pain and organ damage |
| Symptoms Onset | Around 6 months of age |
| Systemic Impact | Affects blood, lungs, bones, eyes, immune system |
| Prevalent Regions | Africa, Mediterranean, Middle East, India, Americas |
| Discovered By |
Dr. James B. Herrick in 1910 |
Latest
How to Live with Sickle Cell
Living with sickle cell disease is about taking back control, not just about putting up with pain. Regular medical checkups, customized drug schedules, and everyday routines can significantly enhance a person’s quality of life.
Patients can avert crises before they begin by drinking plenty of water, avoiding high altitudes, and practicing mindfulness to manage their stress. Being prepared is crucial, much like when you drive on snow tires before winter arrives.
Children benefit most from vaccines and antibiotics because they protect their compromised immune systems. In the meantime, drugs like hydroxyurea are remarkably successful in lowering the incidence of hospital stays and pain episodes.
| Attribute | Description |
|---|---|
| Daily Habits | Stay hydrated, sleep well, eat healthy, avoid stress |
| Exercise Advice | Light to moderate physical activity with caution |
| Medication | Hydroxyurea, folic acid, L-glutamine, pain relievers |
| Monitoring | Regular blood tests, organ function checks |
| Infection Prevention | Vaccinations, antibiotics (especially for children) |
| Pain Management | Personalized pain plans using medications and therapies |
| Mental Health | Stress-reduction techniques, counseling, peer support |
| Helpful Tools | Mobile apps for medication reminders and hydration tracking |
| Support System | Specialized sickle cell centers, patient advocacy groups |
| Lifestyle Goal | Empowered self-management for long-term quality of life |
How Do Sickle Cell Patients Die?

Even though the condition is now much easier to manage, complications can still be fatal. The most common cause of death is still infection, particularly sepsis, which quickly overwhelms the body’s defenses.
Another offender that is frequently mistaken for pneumonia is acute chest syndrome. It causes extreme inflammation and dangerously low oxygen levels by obstructing the lungs’ blood supply with sickled cells.
Organ failure can develop subtly until a crisis arises, especially when it affects the kidneys, liver, or spleen. Another high-risk factor is stroke, which is brought on by vascular blockages that stop blood flow to the brain, particularly in young patients.
| Complication | Description | Risk Level |
|---|---|---|
| Infection | Sepsis, pneumonia, meningitis | Extremely high |
| Acute Chest Syndrome | Lung blockage/infection | Leading cause of hospitalization |
| Stroke | Brain blood flow obstruction | Common in children |
| Organ Failure | Kidneys, liver, spleen affected | Progressive and fatal if unmanaged |
| Pulmonary Hypertension | High blood pressure in lungs | Associated with heart failure |
| Splenic Sequestration | Sudden pooling of blood in spleen | Rapid drop in hemoglobin |
| Blood Clots | Deep vein thrombosis, embolism | Can cause heart attack or stroke |
| Pain Crisis | Unmanaged vaso-occlusive pain | Can escalate to multi-organ failure |
| Pregnancy Complications | Miscarriage, preeclampsia | High-risk for mothers and infants |
| Silent Stroke | No outward symptoms | Long-term brain damage, unnoticed |
What Should Sickle Cell Patients Avoid?
Knowing what not to do can be just as crucial for anyone with this illness as knowing what to do. Common triggers include emotional stress, exposure to cold or extreme heat, and strenuous exercise without adequate hydration.
The sickle cell body must be handled carefully, much like a brittle bridge under stress. Poor sleep patterns, smoking, alcohol, and high altitudes can all make symptoms worse, and infections can be dangerous because they impair spleen function.
Limit processed foods, especially those that are high in unhealthy fats or sodium. Healthy red blood cell production is aided by a diet high in nutrients, and blood circulation is maintained by drinking plenty of water.
| Attribute | Avoidance Area | Why It Matters |
|---|---|---|
| Dehydration | Inadequate fluid intake | Triggers sickling and pain crises |
| Extreme Temperatures | Hot/cold exposure | Causes blood vessel constriction |
| High Altitudes | Mountains, flights | Lower oxygen levels intensify symptoms |
| Strenuous Exercise | Excessive exertion | Increases oxygen demand, risk of crisis |
| Smoking | Cigarettes, vaping | Linked to acute chest syndrome |
| Alcohol | Especially in excess | Leads to dehydration and liver strain |
| Stress | Emotional, physical | Can initiate vaso-occlusive episodes |
| Raw/Undercooked Foods | Meat, eggs | Heightened risk of foodborne illness |
| Poor Sleep | <6 hours/night | Weakens immune response, increases fatigue |
| Missed Medications | Skipping doses | Undermines treatment effectiveness |
Can Sickle Cell be Cured?

Currently, the response is a cautiously positive “yes.” Despite the risks, some patients have been successfully cured by bone marrow transplants, particularly younger patients who had matched sibling donors. Gene therapies that promise a cure, such as Lyfgenia and Casgevy, are especially creative solutions.
Reprogramming the patient’s own stem cells to produce healthy hemoglobin is how these treatments function. Doctors are rewriting genetic instructions using this innovative technique, which is similar to repairing a corrupted file and reinstalling a stable version.
The catch? It’s accessible. Many regions of the world are unable to access these treatments due to their high cost and need for sophisticated healthcare infrastructure.
| Cure Type | Description | Availability |
|---|---|---|
| Bone Marrow Transplant | Replaces diseased marrow with healthy donor marrow | Requires matched donor, mostly children |
| Stem Cell Therapy | Uses patient’s own cells after gene correction | Available in clinical centers |
| Gene Therapy (Casgevy, Lyfgenia) | Edits DNA to increase fetal hemoglobin or fix beta-globin gene | FDA-approved, expensive |
| CRISPR Technology | Cuts faulty DNA and replaces it with healthy code | Revolutionizing treatment pathways |
| Risks | Infection, immune rejection, long-term toxicity | Managed in advanced settings |
| Barriers | Cost, donor availability, hospital access | Slowly improving with global awareness |
| Success Rate | 80–90% in eligible candidates | Higher in children and early intervention |
| Next Steps | Scale accessibility, reduce costs, expand trials | Global initiatives in motion |
How Long can you Live with Sickle Cell Anemia?
The days of a diagnosis implying childhood death are long gone. People with sickle cell anemia now frequently survive into their 50s and beyond in developed countries. Some people continue to lead active, fulfilling lives well into their seventies.
Access to contemporary treatments, regular care, and early diagnosis are all critical components of life expectancy. Similar to managing diabetes or asthma, regular checkups, individualized care, and a dedication to health are crucial.
Many people not only survive but flourish when proactive management is used, pursuing careers, starting families, and giving back to their communities.
| Region | Average Life Expectancy | Notes |
|---|---|---|
| United States | 43–50 years | Increasing with better care |
| United Kingdom | 60–67 years | Access to NHS genetic care |
| Sub-Saharan Africa | <5 years (without care) | Early death due to infections, lack of access |
| With Modern Treatments | 70+ years possible | Seen in patients with proactive self-care |
| Childhood Survival | >95% in developed nations | Thanks to newborn screening and early intervention |
| Key Influencing Factors | Early diagnosis, access to care, therapy adherence | Lifestyle plays a major role |
| Positive Predictors | Regular transfusions, hydroxyurea, gene therapy access | Reduce complications significantly |
| New Outlook | From “lethal” to “livable” | Encouraging progress in treatment and advocacy |
| Hope for the Future | Universal cure by 2030? | WHO and global NGOs aiming for breakthroughs |
What Are the Different Types of Sickle Cell Disease?
Sickle cell disease (SCD) is a collection of hereditary blood disorders that impact hemoglobin rather than a single illness. The production of aberrant hemoglobin, known as hemoglobin S, which under some circumstances causes red blood cells to take on a sickle or crescent shape, is a common feature of these disorders. The combination of inherited hemoglobin gene mutations determines the particular form of sickle cell disease that an individual has.
Sickle cell anemia (HbSS), for example, is the most severe and well-known type and is brought on by a person inheriting the hemoglobin S gene from both parents. Hemoglobin S beta-thalassemia, hemoglobin SC disease, and less common varieties like hemoglobin SD or SE are additional types. Although the symptoms and severity of each type vary, they can all result in major side effects like organ damage, anemia, and pain episodes. Understanding these differences makes it easier to customize management and treatment strategies.
| Type | Description |
|---|---|
| HbSS (Sickle Cell Anemia) | The most severe form, caused by inheriting two sickle cell genes. |
| HbSC | Results from one sickle cell gene and one gene for hemoglobin C, leading to milder symptoms. |
| HbS Beta-Thalassemia | A combination of a sickle cell gene and a beta-thalassemia gene, varying in severity. |
| Rare Variants (HbSD, HbSE) | Caused by combinations of sickle cell and other hemoglobin mutations, generally less common. |
How Is Sickle Cell Anemia Inherited?
Sickle cell anemia is inherited in an autosomal recessive manner. This implies that for a child to get the illness, they need to inherit one faulty hemoglobin S gene from each parent. A child born to parents who have the sickle cell trait (HbAS) has a 25% chance of inheriting two sickle cell genes (HbSS), which can lead to sickle cell anemia.
On the other hand, there is a 25% chance that their child will inherit two normal hemoglobin genes and a 50% chance that their child will inherit one sickle cell gene and one normal gene, making them a carrier with negligible symptoms. This pattern of inheritance emphasizes the value of genetic counseling, especially for people living in areas or populations where sickle cell trait is more common.
| Parent 1 Hb Type | Parent 2 Hb Type | Possible Offspring Outcomes |
|---|---|---|
| HbAS (Trait) | HbAS (Trait) | 25% HbSS (Disease), 50% HbAS (Trait), 25% Normal |
| HbAS (Trait) | Normal (HbAA) | 50% HbAS (Trait), 50% Normal |
| HbAS (Trait) | HbSS (Disease) | 50% HbSS (Disease), 50% HbAS (Trait) |
| HbSS (Disease) | Normal (HbAA) | 100% HbAS (Trait) |
How Common Is Sickle Cell Anemia?

One of the most prevalent genetic diseases in the world, sickle cell anemia is especially prevalent in sub-Saharan Africa, India, the Middle East, and some regions of the Mediterranean. An estimated 100,000 people in the US are thought to have sickle cell disease, and one out of every 365 African-American children is born with the illness.
Millions of people worldwide possess the sickle cell trait, and according to the World Health Organization, areas where malaria was once common have the highest carrier rates. This is because the sickle cell trait helps explain why severe malaria persists in these populations by providing some protection against it. Although life expectancy and quality of life for those afflicted have increased due to public health initiatives, newborn screening programs, and improved treatment options, the disease is still a major global health concern.
| Region | Approximate Prevalence |
|---|---|
| Sub-Saharan Africa | Up to 2% of all newborns; 10–40% of population are carriers. |
| United States | About 100,000 people; 1 in 365 African-American births. |
| India | High prevalence in tribal and some rural populations. |
| Mediterranean | Lower prevalence, but still significant in certain areas. |
What’s the Difference Between Sickle Cell Anemia and Sickle Cell Disease?
All conditions where a person’s red blood cells can sickle because of aberrant hemoglobin are collectively referred to as sickle cell disease (SCD). The most severe type of sickle cell disease, known as sickle cell anemia, is caused by a person inheriting two sickle cell genes (HbSS). To put it another way, not everyone who has sickle cell disease also has sickle cell anemia, even though everyone who has sickle cell anemia also has sickle cell disease.
HbSC, HbS beta-thalassemia, and less common combinations of hemoglobin mutations are additional types of sickle cell disease. The severity, frequency of complications, and methods of treatment of these conditions vary. Patients and healthcare professionals can discuss diagnosis and treatment more accurately when both parties are aware of the difference.
How Is Sickle Cell Anemia Diagnosed?
A blood test is usually the first step in diagnosing sickle cell anemia. Newborns in many nations undergo a routine blood test soon after birth to screen for the disease. Hemoglobin electrophoresis, a test that distinguishes between various forms of hemoglobin, can be used to confirm a diagnosis for people who were not screened at birth.
High-performance liquid chromatography (HPLC) and DNA analysis are additional diagnostic methods that can identify the precise genetic mutations at play. In addition to verifying the existence of sickle cell anemia, these tests can assist in distinguishing it from other types of sickle cell disease or associated hemoglobin disorders. Implementing treatment plans that lower complications and enhance quality of life requires an early and precise diagnosis.
| Test Type | Purpose |
|---|---|
| Newborn Screening | Early detection shortly after birth. |
| Hemoglobin Electrophoresis | Identifies specific hemoglobin types. |
| HPLC | Confirms the presence of HbS and other variants. |
| DNA Analysis | Determines precise genetic mutations. |
Plinko CZ
1xbet يتيح المراهنات المباشرة على المباريات.
1xbet يحتوي على مجموعة كبيرة من ألعاب الكازينو.
After a difficult day, especially one associated with constant stress and physical fatigue, it’s important to be able to relax. Some find peace in meditation or walking, while others rely on digital solutions that create an atmosphere of relaxation and tranquility. On
paczaizm.pl, you can learn how modern platforms help you reconnect, recharge, and unwind using music, videos, or interactive relaxation apps. These technologies are an excellent complement to traditional self-care practices.
The key is to remember that mental and physical health are interconnected. Proper rest not only helps restore strength but also strengthens the body’s resilience. Just as modern treatments for sickle cell anemia restore hope, simple digital relaxation techniques restore inner balance and confidence in the future.
Yüksek kazanç potansiyeli sunan Aviator oyna, heyecanı dorukta yaşamak isteyenler için birebirdir.